The team of Prof. Xiaomin Zhang and Weijia Kong found the interaction of HbA1c and genetic susceptibility on the risk of hearing loss
Type 2 diabetes (T2D), a metabolic disorder characterized by high fasting glucose and insulin resistance, the adverse sequelae of diabetes include macrovascular complications, such as cardiovascular disease, and microvascular complications such as hearing loss (HL) (1). HL, the third leading cause of disability in Global Burden of Disease, developed in 1.57 billion people by 2019, and is estimated to increase to 2.45 billion by 2050 (2,3). As an age-related disease influenced by both genetic and environmental factors, it is worth considering the significance of further research in exploring whether genetic factors and glycemic traits such T2D jointly increase the risk of HL and its severity.
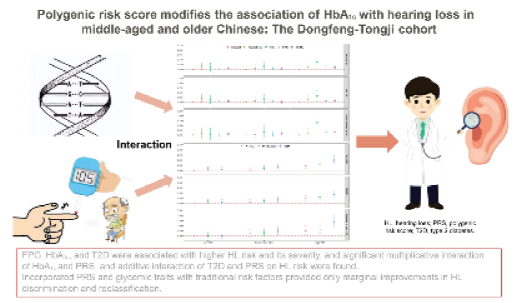
On May 10, 2024, an original study entitled "Polygenic Risk Score Modifies the Association of HbA1c With Hearing Loss in Middle-Aged and Older Chinese: The Dongfeng-Tongji Cohort" was published online in Diabetes Care, an authoritative journal in diabetes. This study, led by the team of Prof. Zhang from the School of Public Health and Prof. Kong from the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, is the first to assess the interactions between genetic susceptibility and fasting plasma glucose (FPG) or glycosylated hemoglobin (HbA1c) levels or T2D in relation to the risks of HL. Based on the Dongfeng-Tongji cohort, this study found multiplicative interactions of HbA1c and PRS on HL risk and its severity, while T2D and PRS had an additive interaction on the HL risk.

After excluding participants missing information on audiometric testing, covariates and genotype data, 13,275 participants from the DFTJ first follow-up survey in 2013 were included in the final analyses. HL was defined as a pure tone average (PTA) >25 dB in the better ear at 0.5, 1, 2, and 4 kHz frequencies, and its severity was further classified as normal (PTA ≤25 dB), mild (PTA 25 to ≤40 dB), and moderate to severe (PTA >40 dB). Prediabetes and T2D were defined based on the 2013 criteria from the American Diabetes Association. A PRS, as a proxy quantifying and summarizing the level of complex genetic risk, was derived from 37 single-nucleotide polymorphisms associated with HL derived from the largest and most recent genome-wide association meta-analysis. Multivariable logistic regression models were fitted to estimate the associations of PRS and glycemic traits (FPG, HbA1c, prediabetes and T2D) with HL risk and its severity. This study assessed the multiplicative interactions between PRS and glycemic traits, as well as the joint associations and additive interactions of PRS with T2D on the HL risks and its severity.
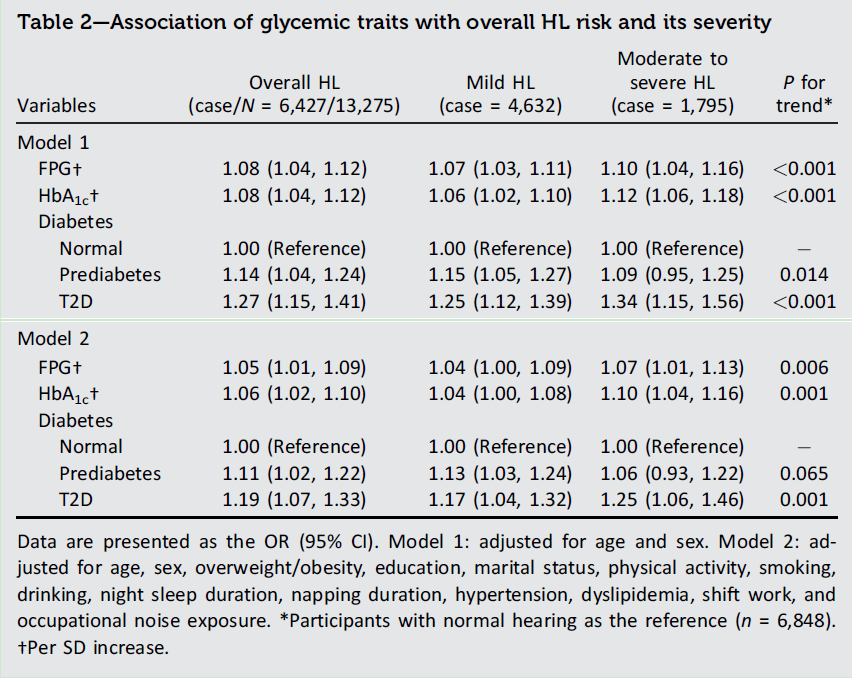
Among the 13,275 participants aged 64.9 years in this study, participants with normal, mild, and moderate to severe HL were 6,848 (51.6%), 4,632 (34.9%), and 1,795 (13.5%), respectively. Increasing FPG and HbA1c levels were strongly associated with higher risks of HL in a linear dose-response manner. In brief, the risks of moderate to severe HL increased by 7% (95% CI 1,13) and 10% (95% CI 4, 16) per-SD increase in FPG and HbA1c levels, respectively (Table 2). Furthermore, compared with participants with normoglycemia, the adjusted ORs (95% CIs) of overall HL risks in those with prediabetes and T2D were 1.11 (1.02, 1.22) and 1.19 (1.07, 1.33), respectively. The risk of moderate to severe HL was the strongest among participants with T2D, with an estimate (95% CI) of 1.25 (1.06, 1.46).
In addition, an elevated PRS had a linear dose-responsive association with a higher risk of overall HL. When the associations of FPG and HbA1c levels with HL risks and its severity stratified by PRS were investigated (Fig. 1), the per-SD increase in FPG and HbA1c levels for both was linked to a 10% higher risk of overall HL among participants in high PRS group, and the corresponding increases for moderate to severe HL were 17% and 16%, respectively. T2D was also associated with higher HL risk and its severity among participants with high PRS, with OR (95% CI) of 1.40 (1.15, 1.69) for overall HL, 1.31 (1.07, 1.60) for mild HL, and 1.65 (1.26, 2.17) for moderate to severe HL. Besides, significant multiplicative interactions were found between PRS and HbA1c level on the risks of overall HL, mild HL, and moderate to severe HL, while interaction was only found between PRS and FPG level on the risk of moderate to severe HL (P for interaction < 0.05).
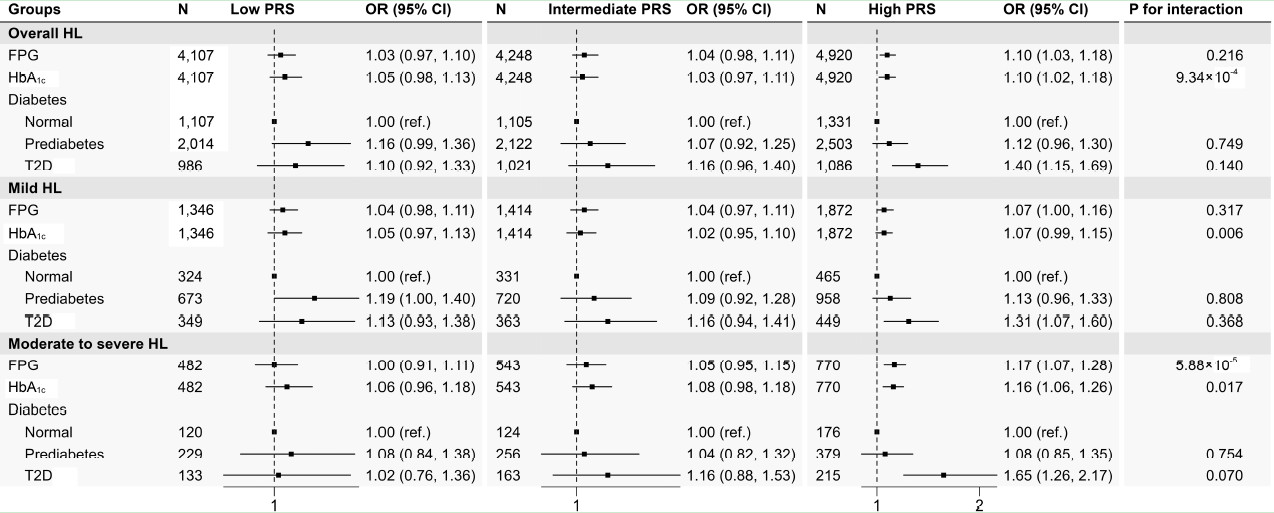
Figure 1—Association of glycemic traits with the risk of HL and its severity stratified by PRS groups.
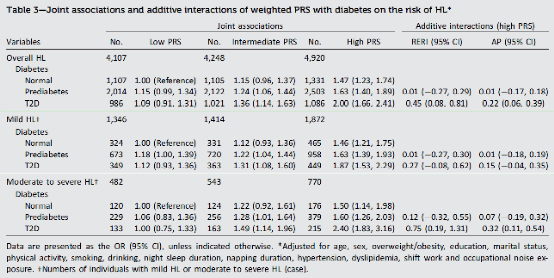
This study also examined the joint associations of the PRS groups with diabetes on the risk of HL and its severity, the estimates of diabetes with HL risks were on the rising trends with the increasing PRS (Table 3). In participants with T2D, the HL risks were the strongest in those in the high PRS group, with an estimate (95% CI) of 2.00 (1.66, 2.41) for overall HL, 1.87 (1.53, 2.29) for mild HL, and 2.40 (1.83, 3.16) for moderate to severe HL. Besides, there was evidence of significant additive interactions between the high PRS and T2D on the overall HL risk.
In summary, our study supports the dose-response associations of HbA1c level with higher HL risk and its severity, and PRS modifies these associations on a multiplicative scale. Additionally, T2D was significantly related to a higher risk of HL, with estimates increasing across HL severity, and a high PRS may interact additively with T2D on HL risk. The findings of our study suggest that management of glycemic traits combined with conventional risk factors might be a better practice to control HL among middle-aged and older adults, especially among those with high susceptibility.
Prof. Xiaomin Zhang from the School of Public Health and Prof. Weijia Kong from the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, are the co-corresponding authors, and PhD student Yaling He is the first author in this work.
Reference
1. Samocha-Bonet D, Wu B, Ryugo DK. Diabetes mellitus and hearing loss: a review. Ageing Res Rev 2021; 71:101423
2. GBD 2019 Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet 2021; 397:996–1009
3. GBD 2019 Ageing Collaborators. Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the Global Burden of Disease 2019 Study. BMJ 2022; 376:e068208